What percentage of US healthcare is publicly funded public opinion unveils a critical examination of America’s complex healthcare landscape, and it’s a story that truly matters. From the very start, you’ll find yourself captivated by the intricate dance of financial support – a delicate balance between public and private contributions. We’ll explore the vast ecosystem of funding, dissecting the roles of government programs, and revealing the latest figures in a clear, digestible format.
It’s a journey through the heart of how healthcare is paid for, setting the stage for a deeper understanding.
But this is more than just a financial breakdown; it’s a look at the human side of healthcare. We’ll delve into the various mechanisms of public funding, such as Medicare, Medicaid, and the Veterans Health Administration, appreciating their unique missions and the communities they serve. Furthermore, we’ll carefully examine public opinion on government involvement in healthcare. You’ll witness how it shifts and changes, influenced by factors like political beliefs and personal experiences, and see how those beliefs shape the debate.
This exploration will lead us to a crucial question: how does all this impact access to healthcare for everyone, and what can we do to make it better?
Understanding the financial architecture of the American healthcare system is essential for context setting
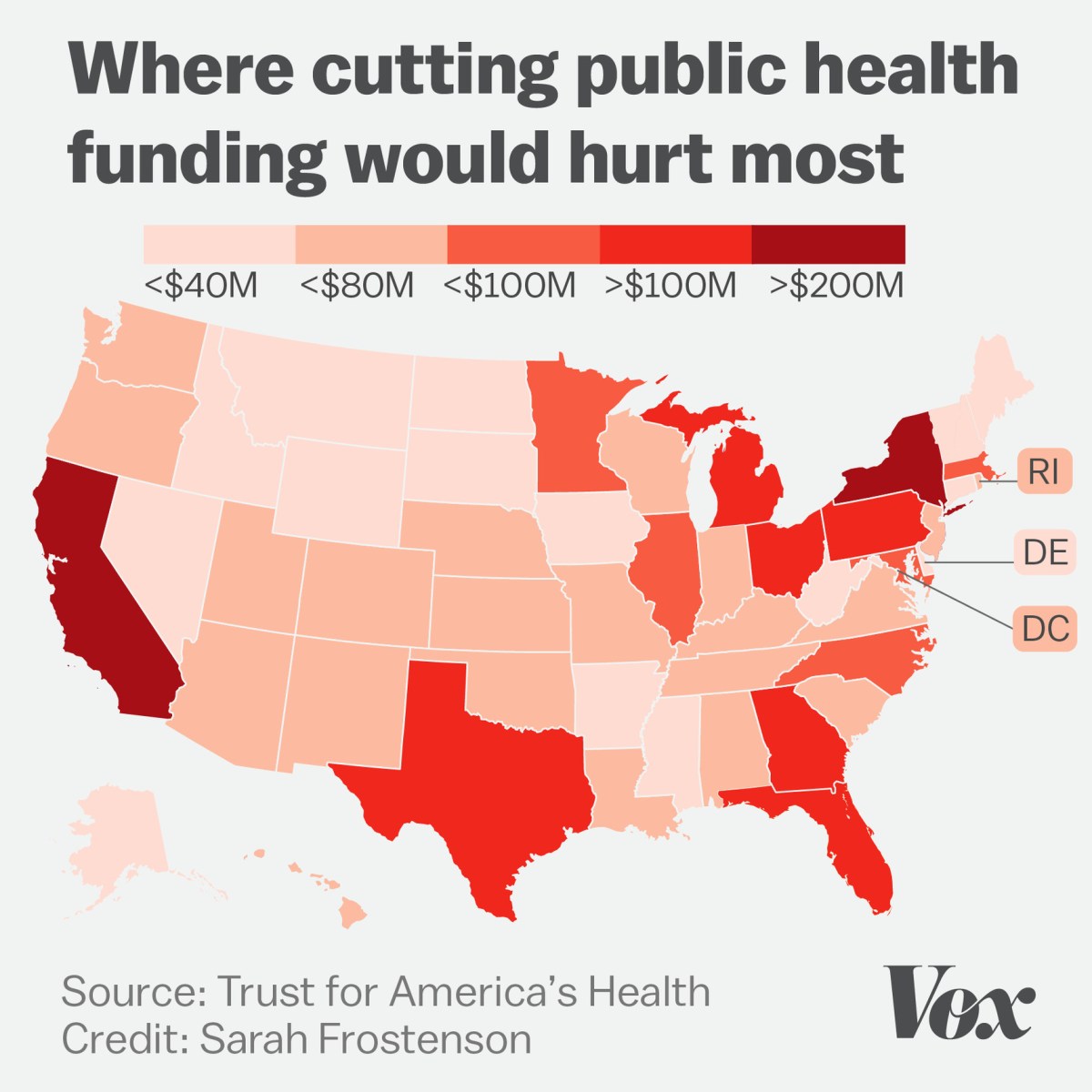
Source: vox-cdn.com
Alright, let’s dive into the fascinating, and sometimes perplexing, world of how we pay for healthcare in the U.S. It’s a complex system, but understanding the basics is crucial to appreciating the discussions around healthcare reform and access. Think of it like understanding the ingredients before you bake a cake; you need to know what’s in it to understand the final product.
Healthcare Funding Sources
The American healthcare system is a fascinating mix of public and private funding, each playing a significant role in how healthcare services are financed. This intricate financial web determines who pays for what, the availability of care, and the overall cost of healthcare in the United States.Healthcare funding in the United States comes from a variety of sources, broadly categorized as public and private.
Public funding originates from government sources, while private funding comes from individuals and employers.* Public Funding: This is money provided by the government at the federal, state, and local levels. It’s funded through tax revenue and other government sources.
Medicare
A federal program primarily for individuals aged 65 and older, as well as younger people with certain disabilities and those with end-stage renal disease.
Medicaid
A joint federal-state program that provides health coverage to millions of Americans, including children, pregnant women, parents, seniors, and people with disabilities. Eligibility and benefits vary by state.
CHIP (Children’s Health Insurance Program)
Provides low-cost health coverage to children in families who earn too much to qualify for Medicaid but cannot afford private insurance.
Veterans Affairs (VA)
Provides healthcare services to eligible veterans.
Military Health System
Offers healthcare services to active-duty military personnel, their families, and retirees.* Private Funding: This comes from individuals, employers, and private insurance companies.
Private Health Insurance
Many Americans receive health insurance through their employers or purchase it individually. Premiums, deductibles, and co-pays are the primary sources of funding.
Out-of-Pocket Expenses
Individuals pay directly for healthcare services not covered by insurance, such as deductibles, co-pays, and certain procedures.
Employer Contributions
Employers often contribute a significant portion of the cost of their employees’ health insurance premiums.The funding mix is constantly shifting, influencing access, affordability, and the overall quality of care.The latest data available, typically from the Centers for Medicare & Medicaid Services (CMS), provides the most accurate snapshot of this funding breakdown. The data from 2022, the most recent year with complete data available, highlights the contributions of public and private sources.
It’s important to note that these percentages can fluctuate slightly year to year.Here’s a simplified breakdown, formatted in a responsive HTML table for clarity:“`html
| Funding Source | Percentage of Total Healthcare Spending (2022) | Explanation | Impact |
|---|---|---|---|
| Private Health Insurance | 33.3% | Premiums paid by individuals and employers. | Influences access to a wide range of providers and services, often with varying cost-sharing requirements. |
| Medicare | 21.2% | Federal government program for the elderly and disabled. | Ensures access to care for a significant portion of the population, influencing payment rates for providers. |
| Medicaid | 17.9% | Joint federal-state program for low-income individuals and families. | Provides a safety net for vulnerable populations, significantly impacting state budgets and healthcare access. |
| Other Public (VA, CHIP, etc.) | 11.7% | Includes programs like the VA, CHIP, and other state and local government spending. | Addresses specific needs of targeted populations, influencing healthcare access and service delivery models. |
| Out-of-Pocket | 9.7% | Payments made directly by individuals for healthcare services. | Affects affordability and can create barriers to care, particularly for those with limited financial resources. |
| Other Private | 6.2% | Includes employer contributions to health insurance and other private sources. | Influences the overall cost of healthcare and access to care. |
“`The table provides a clear visualization of the financial landscape. Understanding these proportions is essential for grasping the impact of policy changes, economic fluctuations, and societal shifts on the accessibility and affordability of healthcare.
Investigating the different forms of public healthcare funding requires careful examination

Source: truthout.org
Let’s dive into the heart of how our healthcare system is funded publicly. It’s a complex landscape, but understanding the different avenues of funding is crucial to grasping the challenges and triumphs of healthcare access and affordability. We’ll explore the major players, their roles, and how they shape the healthcare experience for millions.
Different Types of Public Funding Mechanisms
Public healthcare funding in the United States is a tapestry woven from several key programs, each with its unique focus and funding mechanisms. These programs are designed to support specific populations and address particular healthcare needs.
- Medicare: This is a federal program primarily for individuals aged 65 and older, as well as certain younger people with disabilities or end-stage renal disease. Medicare is funded through payroll taxes, general revenues, and beneficiary premiums. It is administered by the Centers for Medicare & Medicaid Services (CMS) and provides coverage for hospital stays (Part A), physician services (Part B), prescription drugs (Part D), and, in some cases, coverage through Medicare Advantage plans (Part C).
- Medicaid: Medicaid is a joint federal-state program that provides healthcare coverage to low-income individuals and families. The federal government provides matching funds to states, which then administer their Medicaid programs. Eligibility criteria and covered services vary by state, but Medicaid generally covers a broad range of services, including doctor visits, hospital stays, and prescription drugs.
- Veterans Health Administration (VHA): The VHA, part of the Department of Veterans Affairs (VA), provides healthcare services to eligible veterans. It operates a network of hospitals, clinics, and other healthcare facilities across the country. The VHA is funded through appropriations from Congress and provides comprehensive healthcare services, including primary care, specialized care, and mental health services.
Eligibility Criteria and Populations Served by Each Major Public Healthcare Program
Each public healthcare program has specific eligibility criteria, ensuring it serves the intended population. These criteria often reflect the program’s goals and the needs of the individuals it aims to support.
- Medicare: Eligibility is primarily based on age (65 or older) or disability status. Individuals must also be U.S. citizens or have been legal residents for at least five years. Certain younger people with disabilities, such as those with end-stage renal disease or amyotrophic lateral sclerosis (ALS), are also eligible.
- Medicaid: Eligibility is primarily based on income and family size. States set their own income limits, but they must comply with federal guidelines. Medicaid also covers certain other populations, such as pregnant women, children, and individuals with disabilities, who meet specific income and resource requirements.
- Veterans Health Administration (VHA): Eligibility is based on military service and discharge status. Veterans who served in active military, naval, or air service and were discharged or released under conditions other than dishonorable are generally eligible. The VHA also prioritizes veterans with service-connected disabilities and those with lower incomes.
Comparative Analysis: Strengths and Weaknesses Regarding Access and Affordability
Let’s consider the strengths and weaknesses of each major public healthcare program, focusing on access and affordability. Each program faces unique challenges and offers distinct advantages in these areas.
Medicare:
- Strengths: Provides access to healthcare for a large population of older adults and people with disabilities. Offers a wide range of covered services.
- Weaknesses: High out-of-pocket costs, including deductibles, co-pays, and premiums, can create financial barriers for some beneficiaries. Prescription drug coverage (Part D) can be complex and expensive.
Medicaid:
- Strengths: Provides comprehensive healthcare coverage to low-income individuals and families, ensuring access to essential services. Offers significant financial assistance, often with minimal or no cost-sharing.
- Weaknesses: Eligibility criteria and covered services vary by state, leading to disparities in access and coverage. Reimbursement rates to providers can be low, potentially limiting access to care.
Veterans Health Administration (VHA):
- Strengths: Provides comprehensive healthcare services tailored to the needs of veterans, including specialized care and mental health services. Offers a coordinated and integrated healthcare system.
- Weaknesses: Access to care can be limited by long wait times, particularly for appointments with specialists. Geographic limitations can make it difficult for some veterans to access VHA facilities.
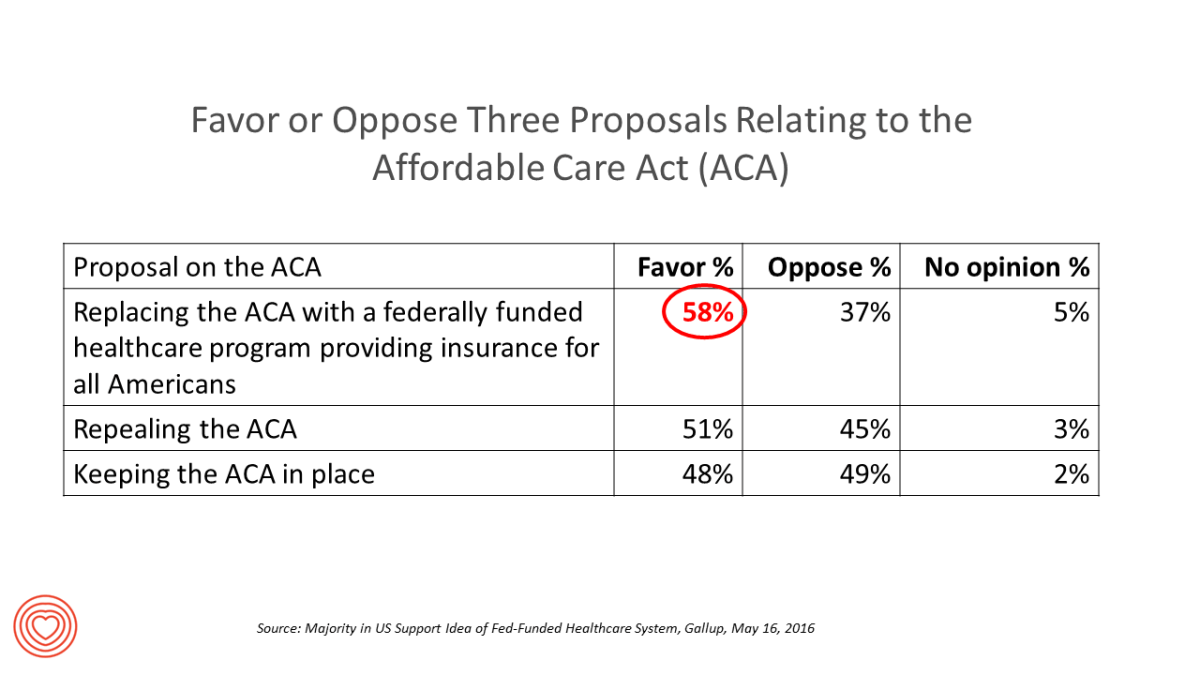
Public opinion towards government involvement in healthcare presents a complex narrative
Navigating the intricate landscape of public sentiment surrounding government’s role in healthcare reveals a tapestry woven with diverse perspectives, shaped by a multitude of influences. Understanding this complexity is crucial for informed discussions and effective policy-making. Public opinion isn’t monolithic; it’s a dynamic entity, constantly shifting in response to evolving societal values, economic realities, and personal experiences.
Current Landscape of Public Sentiment
The current public sentiment regarding government involvement in healthcare is a multifaceted phenomenon. A significant portion of the population supports government intervention, often citing the need for universal access, affordability, and quality control. This viewpoint is frequently associated with the belief that healthcare is a fundamental right, not a privilege. These individuals often advocate for policies like Medicare for All or expansions of the Affordable Care Act (ACA) to ensure everyone has access to necessary medical services.Conversely, another segment of the public expresses reservations about extensive government involvement.
Their concerns typically revolve around potential inefficiencies, increased taxes, and limitations on individual choice. They often prefer a more market-driven approach, believing that competition among private insurers and providers can lead to better quality and lower costs. This perspective frequently emphasizes individual responsibility and the role of the free market in healthcare delivery.There’s also a substantial group that holds a more nuanced view.
They acknowledge the need for some government intervention, such as regulating the insurance market and providing assistance to vulnerable populations, but they are wary of overly broad government control. They often favor a hybrid approach, balancing government oversight with market-based solutions. This middle ground often supports policies that aim to improve healthcare affordability and access while preserving some degree of consumer choice and market competition.
This viewpoint is often represented by those who support the ACA but also want to see improvements to it.
Factors Influencing Public Opinion
Several factors significantly influence public opinion on healthcare. These elements intertwine, creating a complex interplay of individual beliefs and societal trends.* Political Affiliation: Political affiliation is a powerful predictor of healthcare attitudes. Democrats generally favor more government involvement, while Republicans tend to prefer less. This division reflects differing ideological perspectives on the role of government and the nature of healthcare.
For instance, Democrats often support the expansion of Medicaid, while Republicans may advocate for repealing or replacing the ACA.* Socioeconomic Status: Socioeconomic status plays a crucial role. Individuals with lower incomes and limited access to healthcare often support government intervention to ensure affordability and access. Those with higher incomes and comprehensive private insurance may be more likely to oppose government involvement, viewing it as a threat to their existing coverage and potentially leading to higher taxes.* Personal Experiences: Personal experiences with the healthcare system have a profound impact.
Individuals who have faced financial hardship due to medical bills or who have struggled to access necessary care are more likely to support government intervention. Conversely, those who have had positive experiences with private insurance or who are satisfied with their current healthcare arrangements may be less inclined to favor government involvement.* Media Consumption and Information Sources: The media landscape and the sources individuals rely on for information also shape their views.
Exposure to different media outlets, with varying perspectives on healthcare, can significantly influence opinions. For example, someone who primarily consumes news from sources that criticize government healthcare may be more skeptical of government intervention.* Age and Generational Differences: Different age groups may have varying perspectives. Younger generations, who are more likely to have grown up with the ACA and concerns about healthcare affordability, may be more supportive of government intervention.
Older generations, who may be more familiar with the pre-ACA healthcare system, may hold different views.
Evolution of Public Opinion Over Time
Public opinion on government involvement in healthcare has undergone significant shifts over time, influenced by key events and policy changes. The timeline below illustrates this evolution:* 1965: Medicare and Medicaid Established: The creation of Medicare and Medicaid marked a pivotal moment, demonstrating a significant expansion of government involvement in healthcare. This initial expansion was met with considerable debate, but it also laid the groundwork for future discussions about government’s role.
Public opinion was initially divided, with strong support from older adults and low-income individuals, and some resistance from those concerned about increased taxes and government control.* 1980s-1990s: Rise of Managed Care: The rise of managed care organizations, such as HMOs and PPOs, introduced new complexities to the healthcare landscape. Public opinion shifted as consumers faced restrictions on choice and concerns about the quality of care.
This era saw increased scrutiny of insurance companies and calls for greater consumer protections.* 2000s: Debate over Prescription Drug Benefits: The debate over prescription drug benefits, particularly for seniors, intensified. This led to the passage of the Medicare Modernization Act of 2003, which included a prescription drug benefit. Public opinion varied, with support for the benefit but also concerns about its complexity and cost.* 2010: Affordable Care Act (ACA) Enacted: The passage of the ACA was a watershed moment.
The ACA aimed to expand health insurance coverage and reform the insurance market. Public opinion was sharply divided along political lines, with Democrats largely supporting the law and Republicans largely opposing it.* 2017-Present: Ongoing Debates and Challenges: The ACA’s implementation faced ongoing challenges, including efforts to repeal and replace the law. Public opinion continued to evolve, with some Americans benefiting from the law and others facing increased premiums.
The COVID-19 pandemic further highlighted the importance of healthcare access and affordability, leading to renewed discussions about the role of government. The pandemic also illustrated the vulnerability of the healthcare system to public health crises.
The relationship between public funding and healthcare access is crucial for understanding
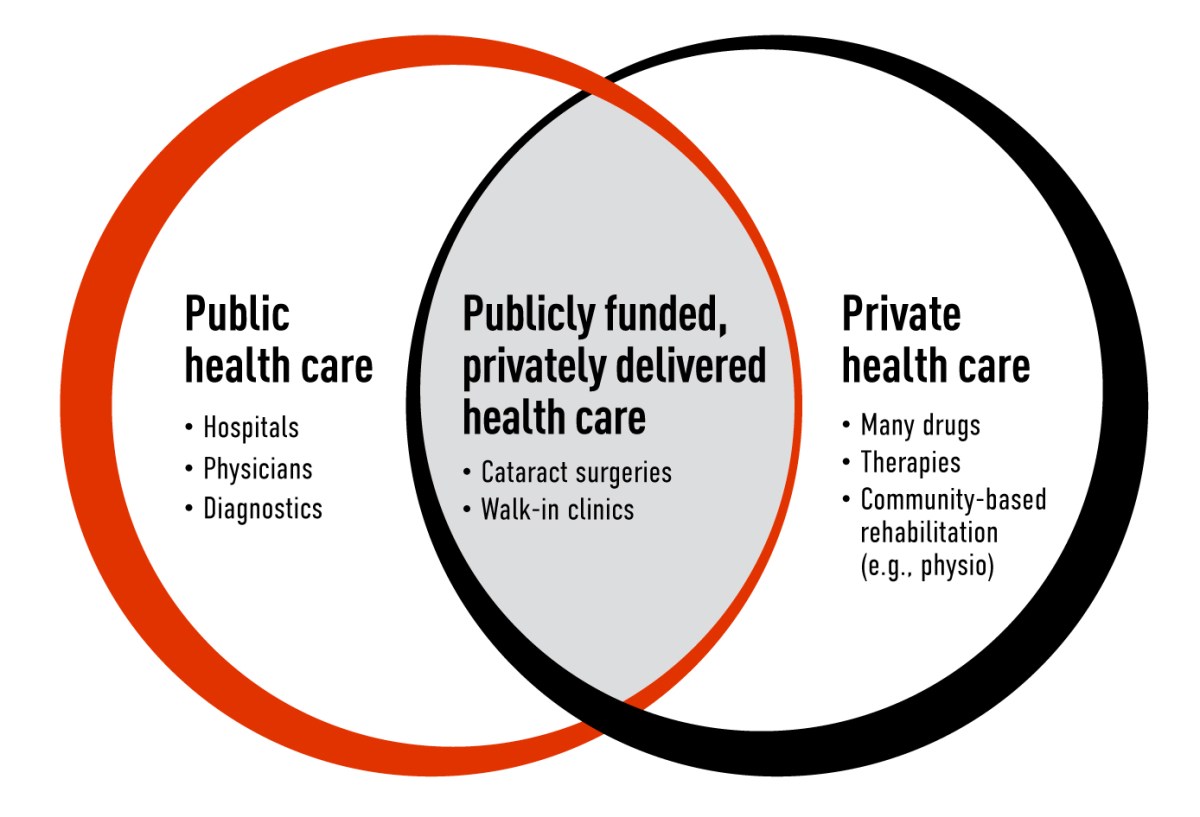
Source: cma.ca
Alright, let’s get real about something super important: how the money flows in healthcare directly affects who gets what kind of care. It’s not just about numbers; it’s about people – their health, their lives, and their ability to thrive. Understanding this connection is key to making things better for everyone.
Public Funding’s Impact on Healthcare Access
Public funding plays a massive role in who can see a doctor, get treatment, and stay healthy. The more money a government puts into healthcare, the more accessible it generally becomes. This is a straightforward relationship, though it’s often muddied by other factors. When public funding is robust, it can significantly lower the cost of care, making it affordable for low-income individuals and families who might otherwise delay or forgo necessary medical attention.
Think about it: less money spent on healthcare means more money for food, housing, and education – the building blocks of a healthy life. Conversely, insufficient public funding often leads to restricted access. This can mean longer wait times for appointments, fewer available services, and a greater reliance on emergency rooms for primary care, which is always a bad situation.The impact varies widely across different groups.
For example, children and the elderly often benefit greatly from publicly funded programs like Medicaid and Medicare, which provide comprehensive coverage that might be otherwise unattainable. Similarly, individuals with disabilities or chronic illnesses depend on public funding to manage their conditions and maintain their quality of life. Without it, these populations would face catastrophic financial burdens and severely limited access to essential care.
However, the level of public funding isn’t just a matter of dollars and cents; it also shapes the types of services available. Public funding can be directed towards preventive care, such as vaccinations and screenings, which helps to catch problems early and prevent more serious (and expensive) conditions down the road. It can also support mental health services, substance abuse treatment, and other often-overlooked areas of healthcare.
Disparities in Healthcare Access
Unfortunately, the playing field isn’t level. Disparities in healthcare access are stark and often reflect deep-seated societal inequalities. These disparities can be seen across racial, ethnic, and geographic lines.
- Race and Ethnicity: People of color frequently face significant barriers to accessing quality healthcare. For instance, African Americans often experience higher rates of chronic diseases like diabetes and heart disease, coupled with lower rates of preventive care and early detection. This is often compounded by factors like systemic racism, implicit bias in healthcare settings, and a lack of culturally competent care.
Consider the example of maternal mortality rates, where Black women are disproportionately affected, highlighting the urgent need for targeted interventions and equitable healthcare practices.
- Geographic Location: Where you live can also dictate your access to care. Rural communities frequently lack adequate healthcare infrastructure, including hospitals, specialists, and even primary care physicians. This can lead to longer travel times, limited access to specialized services, and overall poorer health outcomes. For instance, residents in remote areas may have difficulty accessing specialized cancer treatments or mental health services, forcing them to travel long distances for care, adding to the financial and logistical burdens.
Potential Solutions to Improve Healthcare Access
There’s definitely a way to make things better. Here are some steps that could help:
- Policy Recommendations:
- Expand Medicaid eligibility to cover more low-income individuals and families. This would dramatically increase access to care for a significant portion of the population.
- Increase funding for community health centers, which provide essential services to underserved populations, regardless of their ability to pay.
- Implement policies that promote health equity, such as requiring implicit bias training for healthcare providers and addressing social determinants of health, such as access to healthy food and safe housing.
- Community Initiatives:
- Support the development of telehealth services, especially in rural areas, to increase access to specialists and reduce the need for long-distance travel.
- Promote health literacy programs to educate individuals about their health and empower them to make informed decisions about their care.
- Foster partnerships between healthcare providers, community organizations, and local governments to address the unique needs of specific populations.
By investing in these solutions, we can build a healthcare system that is more equitable, accessible, and responsive to the needs of all Americans.
The economic implications of publicly funded healthcare are significant
Source: healthpopuli.com
Let’s delve into the fascinating world of publicly funded healthcare and unpack its economic ramifications. It’s a topic that sparks heated debates, and for good reason! Understanding the economic benefits and drawbacks is key to grasping the complexities of healthcare financing. This discussion will explore the financial landscape, impact on costs, and the crucial role of the healthcare workforce.
Economic Benefits and Drawbacks, What percentage of us healthcare is publicly funded public opinion
Publicly funded healthcare, at its core, aims to ensure healthcare is accessible to all, regardless of their ability to pay. However, this noble goal comes with a complex web of economic consequences.
Looking ahead, the advancements in the future of AI technology trends 2025 are undeniably exciting, promising a transformation across industries. It’s crucial to consider how we’ll manage the complex advanced computer system care information retrieval as AI systems become more integrated. The impact on the economy is significant, particularly in cities like London; understanding the economic development strategy London automation impact is vital.
Furthermore, we must address the evolving landscape of United States Public Health Service healthcare organizations US regulatory changes to ensure ethical and responsible deployment of these technologies. Finally, embracing the future of retail: profitable growth through technology and AI predictions 2030 allows us to envision a more innovative and efficient future for everyone.
- Potential Economic Benefits: Public funding can lead to several positive outcomes. A healthier population is a more productive population. When people can access necessary medical care, they are less likely to miss work due to illness, boosting overall economic output. Consider countries with robust public healthcare systems, such as Canada or the UK, where universal access to care contributes to a healthier and, arguably, more economically vibrant society.
This proactive approach can also lead to early detection and treatment of illnesses, preventing costly hospitalizations and long-term care needs.
- Potential Economic Drawbacks: The flip side reveals potential challenges. Public healthcare systems often require significant upfront investment, which can be a strain on government budgets. This can lead to higher taxes or cuts in other essential public services. Moreover, some argue that government-run systems can be less efficient than private ones, leading to longer wait times for certain procedures and potentially stifling innovation.
The debate often revolves around the balance between accessibility and efficiency.
- Efficiency Considerations: One key aspect of this debate involves efficiency. Public systems might have less incentive to be cost-conscious, leading to overspending. Conversely, private systems, driven by profit motives, might prioritize cost-cutting measures that compromise quality of care. The ideal scenario involves finding a middle ground, where public funding ensures access while incorporating market mechanisms to promote efficiency and innovation.
Impact of Public Funding on Healthcare Costs
The way healthcare is financed profoundly affects its cost. Public funding models have unique impacts on cost control and potential financial challenges.
- Cost Control Measures: Publicly funded systems often employ various cost-control measures. These can include negotiating bulk discounts with pharmaceutical companies, setting fixed prices for medical procedures, and implementing strict budgeting processes. The goal is to control spending and ensure that resources are used efficiently. The success of these measures varies depending on the specific system and its implementation.
- Potential Financial Challenges: Despite cost-control efforts, public healthcare systems can face financial challenges. An aging population, advancements in medical technology, and rising healthcare utilization all contribute to increased costs. If funding doesn’t keep pace with these rising expenses, the system may face deficits, leading to rationing of services, increased wait times, or cuts in other areas.
- Examples of Cost Control: Consider the National Health Service (NHS) in the UK, which uses a combination of centralized budgeting, price controls, and negotiation with pharmaceutical companies to manage costs. Or, compare it to the US Medicare system, which uses a prospective payment system for hospitals to manage costs, but which is still susceptible to rising costs and financial pressures.
Impact on the Healthcare Workforce
Public funding has a significant influence on the healthcare workforce, impacting employment opportunities and the availability of medical professionals.
- Employment Opportunities: Publicly funded healthcare systems often create a substantial number of jobs in the healthcare sector. This includes physicians, nurses, technicians, administrative staff, and support personnel. These jobs can be a significant source of economic activity, particularly in rural or underserved areas.
- Availability of Medical Professionals: Public funding can also affect the availability of medical professionals. In some cases, it can incentivize doctors and nurses to work in underserved areas, where the need is greatest. However, if salaries and working conditions are not competitive, public systems may struggle to attract and retain skilled healthcare professionals.
- Impact of Student Debt: The burden of student debt is a major concern for many medical professionals. Public funding can sometimes help alleviate this burden through loan forgiveness programs or scholarships for those who agree to work in public service. These programs can encourage more students to pursue careers in healthcare and address workforce shortages. Consider the impact of the National Health Service Corps in the US, which provides scholarships and loan repayment to healthcare professionals in exchange for service in underserved areas.
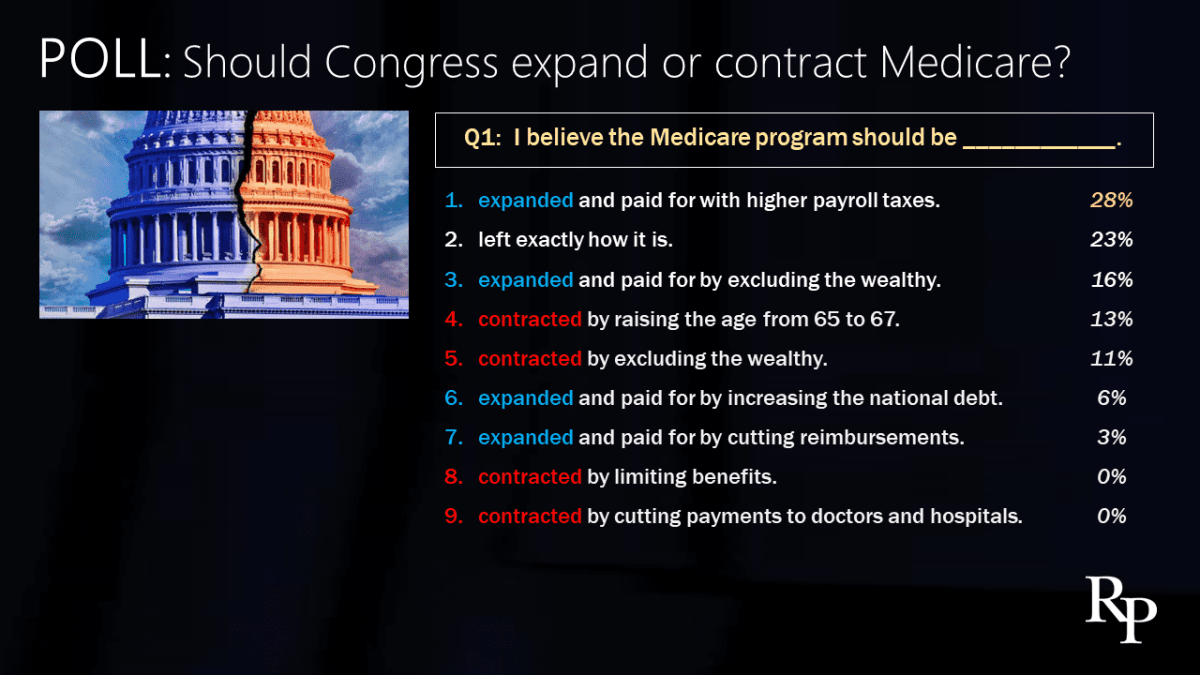
Analyzing the political influences on healthcare funding is a must: What Percentage Of Us Healthcare Is Publicly Funded Public Opinion
The allocation of public funds for healthcare is not a neutral process; it’s deeply intertwined with the ever-shifting landscape of political ideologies and the consequential policy decisions made by those in power. Understanding these influences is critical to grasping the complexities of healthcare financing and its impact on access, quality, and equity. The interplay of political philosophies, partisan agendas, and the powerful voices of lobbying groups significantly shapes how we, as a society, choose to prioritize and fund our healthcare system.
The Role of Political Ideologies and Policy Decisions
Political ideologies form the bedrock upon which healthcare policies are built. Different philosophical perspectives offer contrasting views on the role of government in healthcare, leading to vastly different approaches to public funding. For instance, the debate often centers around the degree of government intervention, the balance between individual responsibility and collective action, and the extent to which healthcare should be considered a right or a privilege.The decisions of policymakers, influenced by their ideological leanings, directly impact the allocation of public funds.
These decisions often involve choices about:
- The Scope of Coverage: Decisions on whether to expand or contract the types of services covered by public funding, such as preventative care, mental health services, or prescription drugs.
- Eligibility Criteria: Defining who qualifies for public assistance, including income thresholds, age restrictions, and other factors.
- Funding Mechanisms: Determining the sources of funding, such as taxes, premiums, or a combination thereof, and the level of funding allocated to specific programs.
- Cost-Control Measures: Implementing strategies to manage healthcare costs, such as price controls, utilization review, or value-based purchasing.
These policy decisions are rarely made in a vacuum. They are shaped by political pressure, economic considerations, and the prevailing public sentiment. The political climate often dictates the feasibility of certain policy proposals, with some ideas gaining traction during periods of economic prosperity and others becoming more appealing during times of crisis. Furthermore, the influence of special interest groups, such as pharmaceutical companies, insurance providers, and physician organizations, can significantly shape the policy landscape.Consider the implementation of the Affordable Care Act (ACA) in the United States.
This landmark legislation, enacted under a Democratic administration, expanded access to health insurance through a combination of subsidies, mandates, and market reforms. However, the ACA faced staunch opposition from Republicans, who argued that it represented excessive government intervention and would lead to higher costs. This ideological divide resulted in ongoing political battles over the law’s implementation and its future. The impact of these political battles on funding, for example, has been visible in states that refused to expand Medicaid, directly limiting access to healthcare for low-income individuals.
Healthcare Policies of Different Political Parties
Comparing the healthcare policies of different political parties reveals stark contrasts in their approaches to public funding and healthcare reform. These differences stem from fundamental disagreements about the role of government and the best ways to ensure access to quality healthcare.
Here’s a comparison:
| Political Party | Approach to Public Funding | Healthcare Reform Goals |
|---|---|---|
| Democrats | Generally support a larger role for government in healthcare, advocating for increased public funding through programs like Medicare and Medicaid. They often favor expanding coverage and providing subsidies to make healthcare more affordable. | Focus on expanding access to healthcare, lowering costs, and improving the quality of care. They often support initiatives such as universal healthcare, expanding the ACA, and negotiating drug prices. |
| Republicans | Generally favor a more limited role for government in healthcare, emphasizing market-based solutions and individual responsibility. They often support tax credits to help individuals purchase insurance and advocate for reducing government spending on healthcare programs. | Focus on reducing healthcare costs, promoting competition among providers, and giving individuals more control over their healthcare choices. They often support repealing and replacing the ACA with alternative market-based reforms. |
These contrasting approaches reflect fundamental differences in ideology. Democrats often view healthcare as a right and believe that the government has a responsibility to ensure access for all. Republicans, on the other hand, often emphasize individual responsibility and believe that market forces can effectively deliver healthcare services. These differences lead to distinct policy proposals, such as the debate over universal healthcare versus market-based reforms.
Impact of Lobbying and Advocacy Groups
Lobbying and advocacy groups exert considerable influence on healthcare policy and funding decisions. These organizations represent a wide range of interests, from pharmaceutical companies and insurance providers to patient advocacy groups and professional medical associations. They employ various tactics to shape policy, including:
- Lobbying: Directly communicating with policymakers to advocate for specific legislation or funding priorities.
- Campaign Contributions: Providing financial support to political campaigns to influence the outcome of elections.
- Public Relations: Conducting public awareness campaigns to shape public opinion and build support for their policy goals.
- Research and Analysis: Funding research and providing data to support their policy positions.
The influence of these groups can be significant. For example, the pharmaceutical industry spends billions of dollars each year on lobbying, advocating for policies that protect their profits, such as patent protection and restrictions on drug price negotiations. Insurance companies also engage in extensive lobbying efforts, seeking to shape regulations that affect their bottom lines. Patient advocacy groups, on the other hand, often advocate for increased funding for research, access to specific treatments, and improvements in patient care.Examples of influential organizations include:
- Pharmaceutical Research and Manufacturers of America (PhRMA): Represents the pharmaceutical industry and lobbies extensively on issues such as drug pricing, patent protection, and research funding. PhRMA’s lobbying efforts have significantly shaped the debate over drug pricing in the United States, influencing the passage of legislation and regulations.
- American Medical Association (AMA): Represents physicians and lobbies on issues such as physician reimbursement, medical liability, and healthcare reform. The AMA’s advocacy has influenced policies related to physician compensation and the structure of the healthcare delivery system.
- American Hospital Association (AHA): Represents hospitals and health systems and lobbies on issues such as hospital funding, regulations, and healthcare policy. The AHA’s lobbying efforts have influenced policies related to hospital reimbursement rates and the provision of healthcare services.
These examples demonstrate the powerful role that lobbying and advocacy groups play in shaping healthcare policy and funding decisions. Their influence can affect the types of healthcare services available, the cost of care, and the overall structure of the healthcare system. Understanding these influences is essential for anyone seeking to navigate the complex world of healthcare finance and policy.
Let’s be honest, the future is now, and it’s powered by AI. Understanding the future of AI technology trends 2025 is crucial, as these advancements will reshape every facet of our lives. To navigate this landscape, we also need to prioritize advanced computer system care information retrieval , ensuring our digital tools remain reliable. This isn’t just about tech; it’s about seizing the opportunities within the economic development strategy London automation impact.
Moreover, the health of our society hinges on the effectiveness of the United States Public Health Service healthcare organizations US regulatory changes. And finally, prepare for a retail revolution, where future of retail: profitable growth through technology and AI predictions 2030 will redefine the consumer experience. Embrace the change, the future is bright!
Comparative perspectives of healthcare funding systems globally can be very informative
Understanding how other countries approach healthcare funding provides invaluable insights for improving our own system. Examining the diverse models employed worldwide, from the single-payer systems to those with mixed funding approaches, offers a roadmap for potential improvements. This comparative analysis highlights the strengths and weaknesses of each approach, allowing for a more informed discussion about the future of healthcare in the United States.
Funding Models Across Nations
The world presents a fascinating array of healthcare funding models, each with its unique characteristics and impact. These systems, though diverse, aim for the same fundamental goal: providing access to quality healthcare for their populations. Let’s delve into some key examples.In Canada, healthcare is primarily funded through a single-payer system. The federal government provides funding to the provinces and territories, which then administer their own healthcare programs.
This model, known as Medicare, ensures that all Canadian citizens and permanent residents have access to medically necessary services, such as hospital care and physician services, without direct out-of-pocket costs at the point of service.The United Kingdom utilizes a National Health Service (NHS), a publicly funded healthcare system. The NHS is primarily funded through general taxation. The NHS provides comprehensive healthcare services, encompassing everything from primary care to specialized treatments.
It emphasizes universal access and equity. The NHS model, though often lauded for its accessibility, faces challenges related to waiting times and resource allocation.Germany’s healthcare system operates on a social insurance model. This system involves a mix of public and private funding. Most Germans are covered by statutory health insurance, funded through contributions from employers and employees. These funds are pooled and managed by sickness funds, which negotiate prices with healthcare providers.
Private health insurance is also available for those who choose to opt out of the statutory system or seek additional coverage.
Healthcare Quality, Access, and Cost-Effectiveness
The outcomes of these different funding models vary significantly, particularly in terms of healthcare quality, access, and cost-effectiveness. A careful comparison of these outcomes reveals both successes and areas for improvement within each system.Regarding healthcare quality, it’s important to acknowledge that measuring this can be challenging. However, indicators such as patient satisfaction, mortality rates for treatable conditions, and the prevalence of chronic diseases can offer insights.
Countries with robust public funding, such as Canada and the UK, often demonstrate good outcomes in these areas, although they may experience challenges related to wait times for specialized procedures. Germany, with its mixed funding approach, often shows high levels of patient satisfaction and access to a wide range of services.Access to healthcare is a crucial aspect of any system.
Single-payer systems, like Canada’s, generally ensure universal access. However, the availability of specialists and certain procedures can be limited. Systems with a mix of public and private funding, such as Germany’s, tend to offer greater choice and access to a wider range of services. The UK, with its emphasis on universal access, has been working to reduce waiting times and improve access to various services.Cost-effectiveness is another key consideration.
The cost of healthcare, as a percentage of GDP, varies significantly across countries. Single-payer systems often have lower administrative costs and greater bargaining power, which can help to control costs. Mixed funding systems may experience higher administrative costs, but they can also foster competition and innovation. The US, with its complex and fragmented system, often struggles with high healthcare costs relative to its outcomes.
Learning from International Best Practices
The U.S. can learn a great deal from international best practices. Adopting elements of successful models from other countries could lead to significant improvements in our healthcare system.One area for potential policy adaptation is the expansion of public insurance coverage. Expanding eligibility for programs like Medicare or Medicaid could improve access to care for millions of Americans. The experiences of Canada and the UK demonstrate the potential benefits of universal coverage.Another area for innovation is price negotiation.
The U.S. could learn from Germany’s system, which allows sickness funds to negotiate prices with healthcare providers. This could help to control costs and make healthcare more affordable.Additionally, investing in primary care and preventive services, as is emphasized in many European systems, can help to reduce healthcare costs in the long run. Early detection and management of chronic diseases can prevent costly hospitalizations and improve overall health outcomes.
“By studying and adapting successful models from around the world, the U.S. can create a healthcare system that is more affordable, accessible, and effective for all its citizens.”
Closing Summary
Source: robertpearlmd.com
In conclusion, we’ve journeyed through the multifaceted world of healthcare funding in the United States. From the intricate financial structures to the passionate opinions of the public, we’ve explored the crucial links between funding, access, and the economic realities that shape our system. Understanding these complexities is the first step towards positive change. By examining international models, we can imagine a future where healthcare is more accessible, affordable, and truly reflects the needs of everyone.
The future of healthcare is a conversation, and it’s a conversation worth having, filled with potential for improvement and innovation.